Education and Healthcare Suck for the Same Reasons: And Here's How We Can Change That
Education and Healthcare Suck for the Same Reasons: And Here's How We Can Change That
Education and Healthcare Suck for the Same Reasons: And Here's How We Can Change That
Nov 30, 2024
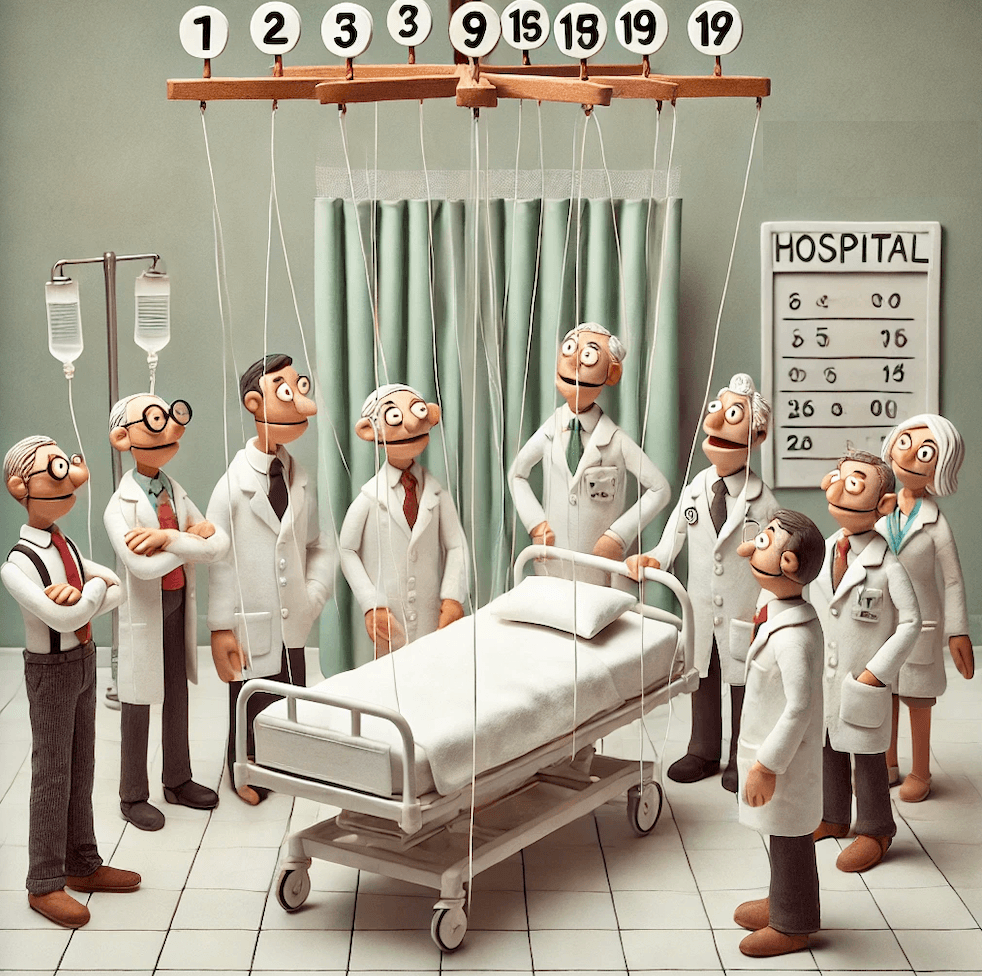
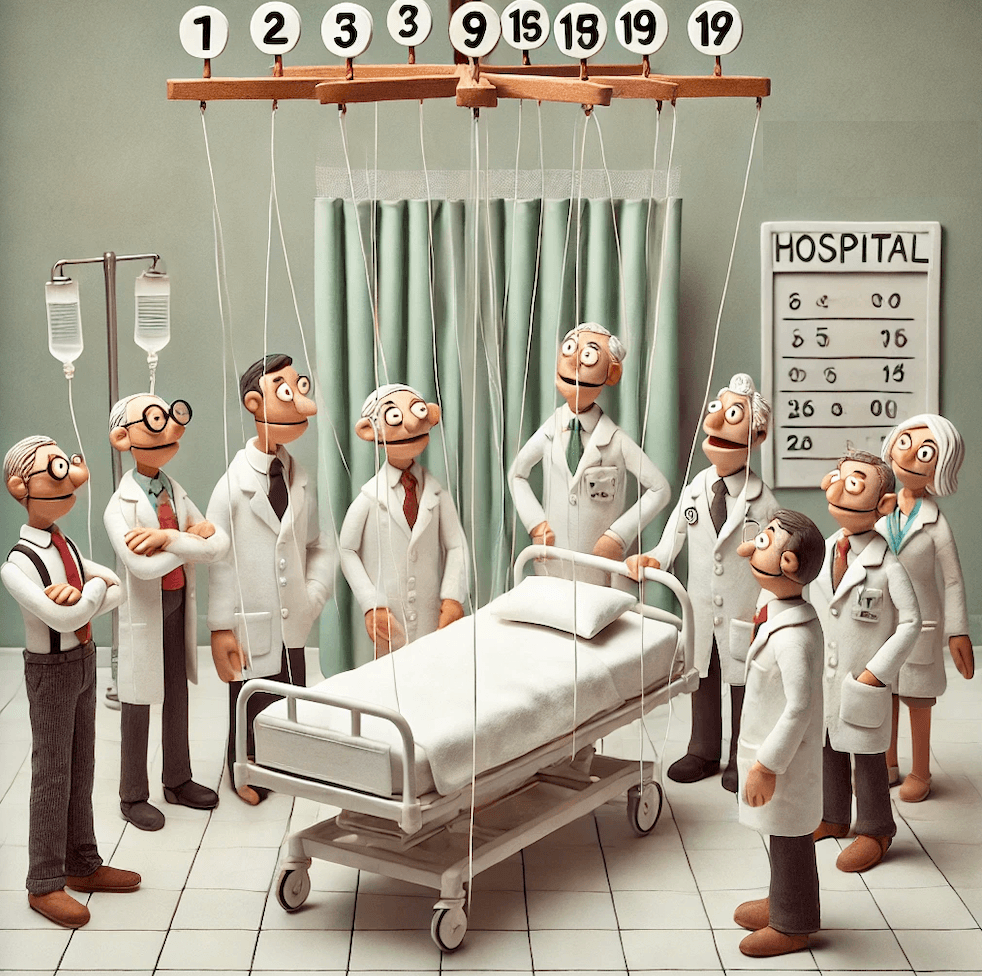
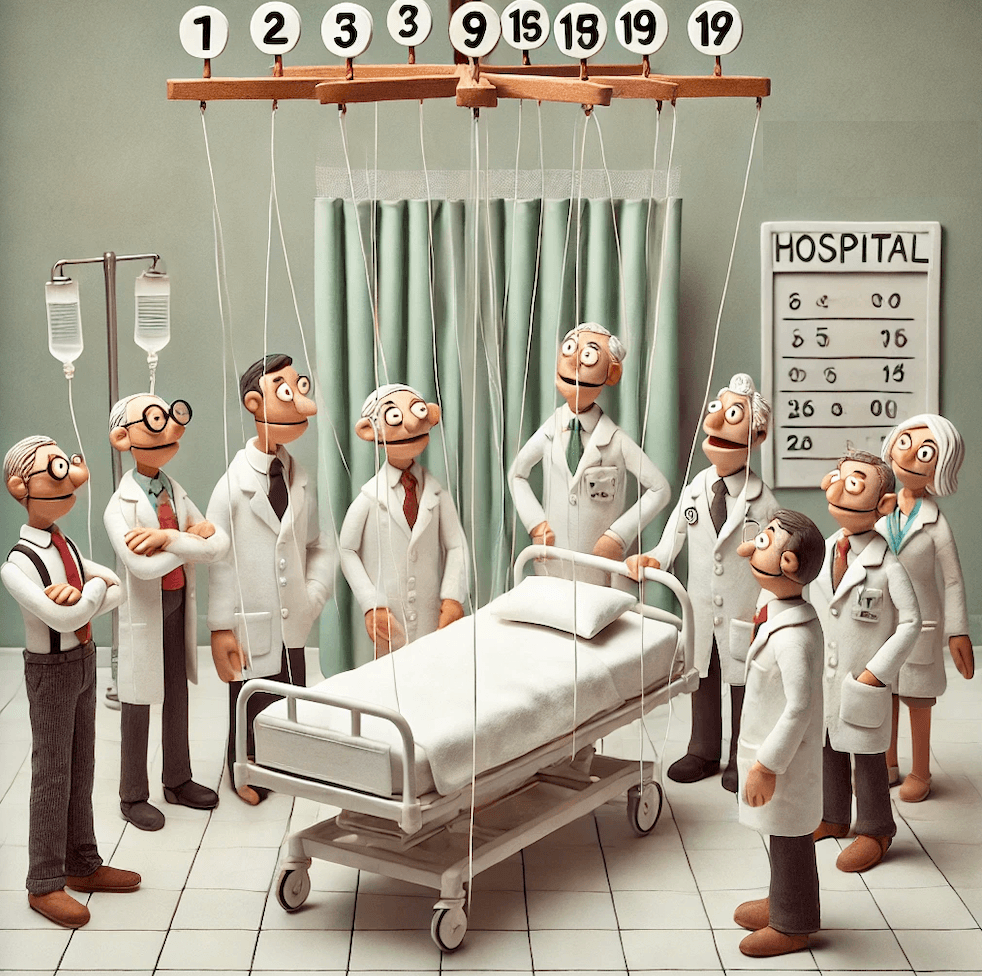
The clock strikes 6 AM in a hospital room. An attendant barges in, disrupting precious sleep to swap out an untouched water jug. Soon after, a parade of nurses follows, each focused on collecting their designated measurements. Blood pressure. Temperature. Oxygen levels. In this flurry of activity, something crucial gets lost – the actual patient.
Miles away, in a classroom, a similar scene unfolds. A teacher moves mechanically through standardized material, focused on test scores and grade averages. Thirty unique minds sit before her, but what exists in the system's eyes are just data points to be measured and tracked. The student, like our patient, has vanished.
These aren't isolated problems. They're symptoms of the same disease: our obsession with measurable outcomes has eclipsed the humans at the center of these systems.
The Tyranny of Metrics
Just as a patient becomes reduced to their vital signs and lab results, students become their test scores and grades. The metrics that were meant to help us understand how well we're doing our jobs – caring for the sick and educating the young – have become the job itself.
This isn't to say measurements aren't valuable. Modern medicine is indeed miraculous. We can view gallstones on high-definition screens and remove them through tiny incisions, sending patients home the next day. Similarly, educational assessments can provide valuable insights into learning progress. But somewhere along the way, we forgot these tools are meant to serve people, not the other way around.
Standardization Gone Wrong
Both healthcare and education faced similar pressures in the 20th century. As knowledge expanded exponentially, systems needed to scale up to serve more people. The solution? Standardization. Create protocols, establish benchmarks, develop universal procedures. It worked – sort of.
Just as the US Air Force discovered in the 1940s that their standardized cockpit fit exactly zero of their pilots perfectly, our standardized approaches to healthcare and education fit no one perfectly. As Todd Rose points out in "The End of Average," designing for the average means designing for no one.
The Business of Caring
Making matters worse, both sectors have become big business. When profit enters the equation, those measurable outcomes take on even more importance – they become tied to revenue. Hospitals optimize for billable procedures rather than patient wellbeing. Schools focus on test scores that attract funding rather than genuine learning.
The Knowledge Gap
What makes both healthcare and education particularly vulnerable to market failures is a fundamental problem: consumers often can't judge what they actually need. When your doctor recommends a battery of tests or your child's school suggests early tutoring, how do you evaluate if these interventions are truly necessary?
This information asymmetry creates a perfect storm for over-servicing. More medications, more diagnostic tests, more coaching classes for ever-younger children – all justified under the banner of "better safe than sorry." The business model thrives on this uncertainty. After all, what parent wouldn't want to give their child every possible advantage? What patient wouldn't want to rule out every possible condition?
Traditional market forces fail spectacularly here because the measures of success are both delayed and difficult to quantify. How do you attribute a child's success ten years later to specific educational choices made in elementary school? How do you measure the long-term impact of preventive healthcare? These outcomes manifest in complex measures of wellbeing and success that no one in the current system has any incentive to track.
The result? A systemic bias toward more – more intervention, more services, more products – regardless of actual need. The market can't efficiently sort good solutions from unnecessary ones when the feedback loop is so long and murky. This isn't just about profit-seeking; it's about the fundamental structure of these markets.
The Way Forward
So how do we fix systems this broken? Here's where we need to start:
Return to First Principles We must reconnect with the fundamental purpose of these institutions. Healthcare exists to help people heal and maintain wellbeing. Education exists to help people learn and grow. Every policy and procedure should be measured against these basic truths.
Embrace Personalization Just as learning must be personalized because there is no "average student," healthcare must be personalized because there is no "average patient." This means creating flexible systems that can adapt to individual needs while maintaining high standards of quality.
Empower the Humans Both doctors and teachers need the autonomy to exercise their professional judgment. When we reduce complex professions to a series of checkboxes and protocols, we lose the human insight that makes these services valuable in the first place.
Rethink Metrics We need more sophisticated ways to measure success. Simple numerical scores – whether test results or patient satisfaction surveys – can't capture the complexity of learning or healing. We need qualitative measures that account for individual circumstances and long-term outcomes.
Build Community-Centered Models Both healthcare and education work best when embedded in communities. The Finnish education system and community health worker programs in developing countries show how this can work. When these services are treated as community resources rather than business units, priorities naturally align with human needs.
The Path to Change
Transformation won't be easy. Entrenched systems resist change, and the current models have powerful defenders. The challenge runs deeper than just resistance to change – it's built into the economic structure itself. The incentives to maintain broad, oversimplified metrics are perverse but profitable. No business will voluntarily build systems that expose their shortcomings or reduce their margins.
This is where we need a radical rethinking of how we fund innovation in these crucial sectors. We need new models where deeply interested people come together to fund and drive change from the ground up. Take ApniPathshala, for instance – they're creating learning pods where children can engage in truly self-directed learning, leveraging the vast resources available online while providing the human guidance and community support essential for real learning.
Similar initiatives could transform healthcare. Imagine community-funded clinics that maintain transparent databases of treatments, outcomes, and patient experiences. These wouldn't just track the usual metrics but would document what's been tried, what's failed, and why – creating a knowledge base that serves people rather than profits.
These systems will never emerge from within current institutional structures because transparency and detailed outcome tracking could hurt profits by highlighting inefficiencies and failures. But that's exactly the kind of insight we need to make outcomes better for everyone.
The way forward lies in open-source initiatives, crowdfunded projects, and collaborative efforts that prioritize human outcomes over institutional metrics. We can build regional adaptations of what works, share knowledge freely, and create networks of care and learning that serve communities rather than shareholders. There already are a few promising initiatives to fund such ideas. We need many more.
We don't need to choose between efficiency and empathy, between standards and personalization. We need systems clever enough to deliver both. The technology exists. The knowledge exists. What we need now is the will to change – and people willing to build and systems to fund these alternatives.
The next time a nurse walks into a patient's room or a teacher faces their class, they should see not just a set of metrics to be measured, but a whole person to be cared for. That's when we'll know we're on the right track.
Interested in being part of this change? Get in touch with us. Yes, it's a challenge – entrenched systems always are. But few challenges are more worthy of our time and effort than reimagining how we care for and educate our communities.
Interested? Please reach out to us!
The clock strikes 6 AM in a hospital room. An attendant barges in, disrupting precious sleep to swap out an untouched water jug. Soon after, a parade of nurses follows, each focused on collecting their designated measurements. Blood pressure. Temperature. Oxygen levels. In this flurry of activity, something crucial gets lost – the actual patient.
Miles away, in a classroom, a similar scene unfolds. A teacher moves mechanically through standardized material, focused on test scores and grade averages. Thirty unique minds sit before her, but what exists in the system's eyes are just data points to be measured and tracked. The student, like our patient, has vanished.
These aren't isolated problems. They're symptoms of the same disease: our obsession with measurable outcomes has eclipsed the humans at the center of these systems.
The Tyranny of Metrics
Just as a patient becomes reduced to their vital signs and lab results, students become their test scores and grades. The metrics that were meant to help us understand how well we're doing our jobs – caring for the sick and educating the young – have become the job itself.
This isn't to say measurements aren't valuable. Modern medicine is indeed miraculous. We can view gallstones on high-definition screens and remove them through tiny incisions, sending patients home the next day. Similarly, educational assessments can provide valuable insights into learning progress. But somewhere along the way, we forgot these tools are meant to serve people, not the other way around.
Standardization Gone Wrong
Both healthcare and education faced similar pressures in the 20th century. As knowledge expanded exponentially, systems needed to scale up to serve more people. The solution? Standardization. Create protocols, establish benchmarks, develop universal procedures. It worked – sort of.
Just as the US Air Force discovered in the 1940s that their standardized cockpit fit exactly zero of their pilots perfectly, our standardized approaches to healthcare and education fit no one perfectly. As Todd Rose points out in "The End of Average," designing for the average means designing for no one.
The Business of Caring
Making matters worse, both sectors have become big business. When profit enters the equation, those measurable outcomes take on even more importance – they become tied to revenue. Hospitals optimize for billable procedures rather than patient wellbeing. Schools focus on test scores that attract funding rather than genuine learning.
The Knowledge Gap
What makes both healthcare and education particularly vulnerable to market failures is a fundamental problem: consumers often can't judge what they actually need. When your doctor recommends a battery of tests or your child's school suggests early tutoring, how do you evaluate if these interventions are truly necessary?
This information asymmetry creates a perfect storm for over-servicing. More medications, more diagnostic tests, more coaching classes for ever-younger children – all justified under the banner of "better safe than sorry." The business model thrives on this uncertainty. After all, what parent wouldn't want to give their child every possible advantage? What patient wouldn't want to rule out every possible condition?
Traditional market forces fail spectacularly here because the measures of success are both delayed and difficult to quantify. How do you attribute a child's success ten years later to specific educational choices made in elementary school? How do you measure the long-term impact of preventive healthcare? These outcomes manifest in complex measures of wellbeing and success that no one in the current system has any incentive to track.
The result? A systemic bias toward more – more intervention, more services, more products – regardless of actual need. The market can't efficiently sort good solutions from unnecessary ones when the feedback loop is so long and murky. This isn't just about profit-seeking; it's about the fundamental structure of these markets.
The Way Forward
So how do we fix systems this broken? Here's where we need to start:
Return to First Principles We must reconnect with the fundamental purpose of these institutions. Healthcare exists to help people heal and maintain wellbeing. Education exists to help people learn and grow. Every policy and procedure should be measured against these basic truths.
Embrace Personalization Just as learning must be personalized because there is no "average student," healthcare must be personalized because there is no "average patient." This means creating flexible systems that can adapt to individual needs while maintaining high standards of quality.
Empower the Humans Both doctors and teachers need the autonomy to exercise their professional judgment. When we reduce complex professions to a series of checkboxes and protocols, we lose the human insight that makes these services valuable in the first place.
Rethink Metrics We need more sophisticated ways to measure success. Simple numerical scores – whether test results or patient satisfaction surveys – can't capture the complexity of learning or healing. We need qualitative measures that account for individual circumstances and long-term outcomes.
Build Community-Centered Models Both healthcare and education work best when embedded in communities. The Finnish education system and community health worker programs in developing countries show how this can work. When these services are treated as community resources rather than business units, priorities naturally align with human needs.
The Path to Change
Transformation won't be easy. Entrenched systems resist change, and the current models have powerful defenders. The challenge runs deeper than just resistance to change – it's built into the economic structure itself. The incentives to maintain broad, oversimplified metrics are perverse but profitable. No business will voluntarily build systems that expose their shortcomings or reduce their margins.
This is where we need a radical rethinking of how we fund innovation in these crucial sectors. We need new models where deeply interested people come together to fund and drive change from the ground up. Take ApniPathshala, for instance – they're creating learning pods where children can engage in truly self-directed learning, leveraging the vast resources available online while providing the human guidance and community support essential for real learning.
Similar initiatives could transform healthcare. Imagine community-funded clinics that maintain transparent databases of treatments, outcomes, and patient experiences. These wouldn't just track the usual metrics but would document what's been tried, what's failed, and why – creating a knowledge base that serves people rather than profits.
These systems will never emerge from within current institutional structures because transparency and detailed outcome tracking could hurt profits by highlighting inefficiencies and failures. But that's exactly the kind of insight we need to make outcomes better for everyone.
The way forward lies in open-source initiatives, crowdfunded projects, and collaborative efforts that prioritize human outcomes over institutional metrics. We can build regional adaptations of what works, share knowledge freely, and create networks of care and learning that serve communities rather than shareholders. There already are a few promising initiatives to fund such ideas. We need many more.
We don't need to choose between efficiency and empathy, between standards and personalization. We need systems clever enough to deliver both. The technology exists. The knowledge exists. What we need now is the will to change – and people willing to build and systems to fund these alternatives.
The next time a nurse walks into a patient's room or a teacher faces their class, they should see not just a set of metrics to be measured, but a whole person to be cared for. That's when we'll know we're on the right track.
Interested in being part of this change? Get in touch with us. Yes, it's a challenge – entrenched systems always are. But few challenges are more worthy of our time and effort than reimagining how we care for and educate our communities.
Interested? Please reach out to us!
Interested in Receiving Updates?
Interested in Receiving Updates?
Interested in Receiving Updates?
BetterSchooling is a resource for Indian families to learn more about alternative schooling and alternative learning tools and resources.
